Magnetic Resonance Imaging (MRI) has revolutionized the field of medical diagnostics, particularly with the advent of functional MRI (fMRI). This sophisticated neuroimaging technique has provided unprecedented insights into brain activity, revealing how cognitive processes correlate with various neuroanatomical phenomena. However, as with any medical intervention, there are questions surrounding the safety and effects of fMRI. Is fMRI bad for your health? Let’s explore the nuances of this captivating technology, assessing its promises and potential risks.
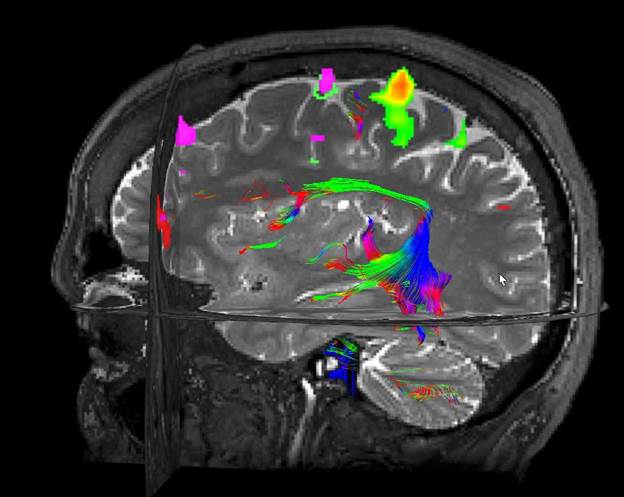
First, we must delineate the mechanism by which fMRI operates. Unlike traditional imaging techniques that rely on ionizing radiation, fMRI utilizes magnetic fields and radio waves to detect changes in blood flow associated with neuronal activity. This approach hinges on the principle of hemodynamic response, where active areas of the brain require increased oxygenation delivered via the bloodstream. The result is a non-invasive tool that enables researchers to observe real-time brain functions during cognitive tasks—a boon for both scientific inquiry and clinical practice.
The implications of fMRI in understanding the human brain are profound. Its capacity to illuminate the intricacies of behaviors, decision-making processes, and even emotional responses has paved the way for advances in psychological and psychiatric treatments. Furthermore, fMRI has established itself as an invaluable resource in pre-surgical mapping, assisting neurosurgeons in navigating areas critical for preserving vital functions while excising pathological tissue.
However, the discourse surrounding the potential health ramifications of fMRI cannot be overlooked. While generally considered safe, there are several factors to consider. One of the primary concerns involves the magnetic field used during imaging. The strong stationary magnetic fields generated in the MRI machine can interact with metallic objects, which raises significant safety issues. Patients with ferromagnetic implants, pace-makers, or certain types of neurostimulators are typically deemed unsuitable candidates for fMRI due to the risk of these objects being affected by the magnetic forces.
Moreover, some individuals exhibit claustrophobia or anxiety when placed within the confines of the MRI scanner. This psychological aspect can trigger physiological stress responses, which, while indirectly related, merit consideration when evaluating the overall health impact of fMRI. To mitigate such adverse effects, practitioners have begun employing innovative techniques such as open MRI systems, which provide a less restrictive environment, allowing for enhanced patient comfort.
Another layer of complexity pertains to the radiofrequency (RF) pulses used during the fMRI process. These RF pulses have raised questions regarding their effects on biological tissues. Current studies indicate that RF exposure is unlikely to have deleterious effects; however, continuous exposure over extended periods remains an area of active investigation. Understanding the long-term implications, particularly in populations with chronic conditions necessitating frequent imaging, is essential for comprehensive risk assessment.
Importantly, we must also consider fMRI’s role in predicting and diagnosing neurodegenerative diseases. Although fMRI does not involve ionizing radiation, the inherent risks associated with prolonged scanning sessions should not be underestimated. As the population ages, rates of neurodegenerative diseases are expected to rise, leading to increased utilization of fMRI in clinical settings. This scenario raises questions about cumulative exposure and the potential for adverse reactions over time.
Yet, the potential benefits of fMRI cannot be relegated to background noise. Numerous studies have demonstrated its success in therapeutic contexts, particularly in discerning the brain’s adaptability—a phenomenon known as neuroplasticity. The ability of the brain to reorganize itself and form new neural connections can be crucial in rehabilitation following strokes or traumatic injuries. Here, fMRI serves to illuminate areas of functional redundancy, guiding targeted therapy that fosters recovery.
Moreover, fMRI continues to be instrumental in elucidating the neurobiological underpinnings of psychiatric disorders, such as depression, anxiety, and schizophrenia. By examining variations in brain activation patterns, researchers can corral data that elucidate pathophysiological processes, allowing for personalized medicine approaches that enhance treatment efficacy. Consequently, the promise of fMRI in advancing our understanding of mental health disorders is both compelling and vital.
While discussing health implications, it is crucial to address the ethical dimensions surrounding neuroimaging technologies. The proliferation of fMRI in both clinical and research settings invites questions about privacy and the potential misuse of brain data. As our understanding of neural correlates of behavior deepens, the ethical ramifications of discerning one’s thoughts or intentions through fMRI can’t be ignored. Society must grapple with which information is shared and how it is utilized, ensuring that this powerful tool serves to enhance human well-being rather than compromise it.
In conclusion, the question of whether fMRI is detrimental to health is not a straightforward one. It requires a balanced examination of both its remarkable contributions to medicine and the potential risks associated with its application. As research continues to illuminate the multifaceted nature of fMRI, it is essential to foster a culture of inquiry that appreciates both the promises and perils of this groundbreaking technology. By doing so, we can advocate for informed decision-making that elevates the ethical standards of neuroimaging, while triumphantly harnessing its capabilities to better understand the enigmas of the human brain.