In the complex interplay between biology and technology, innovative strategies are continuously evolving to address critical health challenges. One compelling area of exploration is the crystallization phase change, a phenomenon that has garnered attention for its potential application in neonatal care. This concept revolves around the manipulation of materials to modify temperature regulation, which could prove life-saving for premature infants. However, can such a scientific approach effectively challenge the current methodologies employed in neonatal intensive care units (NICUs)? This question not only invites inquiry but poses a significant challenge to existing paradigms.
Premature birth—a global concern affecting millions of infants annually—results in numerous health complications, including hypothermia. Infants born before 37 weeks of gestation often have underdeveloped thermoregulatory systems, leaving them vulnerable to dangerously low body temperatures. In NICUs, maintaining optimal environmental temperatures for these neonates is crucial. The standard approach relies heavily on incubators or heated blankets, devices that, while effective, can pose risks such as fluid loss or thermal instability. Consequently, alternative methodologies leveraging phase change materials (PCMs) are being examined for their promising capabilities to enhance neonatal thermal care.
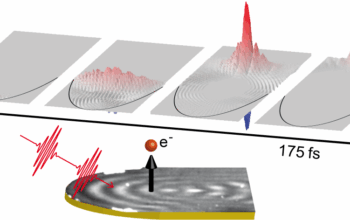
PCMs operate based on their unique ability to absorb and release latent heat during phase transitions—most commonly from solid to liquid and vice versa. This thermal storage mechanism can provide a stable, controllable environment for premature infants, significantly mitigating the challenges posed by traditional heating methods. When integrated into neonatal care, PCMs could offer not only consistent warmth but also reduced energy consumption and minimal maintenance, thus addressing some of the critical limitations of conventional devices.
Consider the scenario where a premature infant is swaddled in a blanket that incorporates a PCM designed specifically for neonatal use. As the infant’s body temperature begins to drop, the PCM absorbs the excess heat, effectively stabilizing the ambient temperature surrounding the infant. Conversely, should the infant’s temperature rise, the PCM would release heat to facilitate cooling. This bidirectional thermal regulation showcases the remarkable adaptability of phase change technology, presenting a significant advancement over traditional, less nuanced approaches.
In addition to conceptualizing and implementing PCMs in neonatal care, researchers are investigating the customization of these materials to cater specifically to neonatal physiology. Integrating biocompatible substances into PCM formulations is imperative to ensuring safety for infants with highly sensitive skin and underdeveloped immune systems. Moreover, enhancing the thermal conductivity of these materials could further improve their efficacy, ensuring that they respond rapidly to temperature fluctuations around the newborn.
However, the venture into phase change materials is not devoid of challenges. While experimental data suggests the efficacy of PCMs in controlled environments, their integration into everyday clinical practice necessitates thorough validation through rigorous clinical trials. One must ponder: What barriers hinder the widespread adoption of this innovative technology? Potential implications for healthcare costs, training of personnel, and regulatory issues all create a landscape rife with complexities.
Furthermore, the introduction of PCMs invites questions surrounding the design and ergonomy of these thermal management solutions. Innovative heating and cooling strategies must seamlessly integrate within existing NICU infrastructures to be truly successful. This requires multidisciplinary collaboration among medical professionals, engineers, and designers to create solutions that are not only technically sophisticated but also user-friendly in high-stress environments.
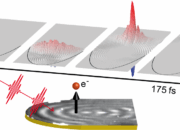
Moreover, while PCMs promise significant advancements, continuous monitoring of infant temperature remains integral. Thus, synergies between PCM technology and digital monitoring systems could enhance the adaptability and responsiveness of care provided in NICUs. Deploying sensors that relay real-time temperature data could enable more precise interventions and ensure that the benefits of PCMs are fully realized.
The exploration of phase change materials in neonatal care exemplifies a broader commitment to merging science with compassion. As research progresses, the ultimate aim remains to enhance the quality of life for the most vulnerable. This endeavor will require comprehensive studies evaluating the long-term effects of PCM usage on premature infants, as well as parent and clinician feedback to continuously improve the innovation. It emphasizes a crucial dimension of healthcare—the necessity for evidence-based strategies, ensuring that compassionate care is equally underscored with scientific validity.
As the realm of neonatal care evolves, the challenge remains for stakeholders to embrace innovative technologies while safeguarding the welfare of infants. The infusion of phase change materials into clinical practice is emblematic of how physics can inform and revolutionize our approaches to health. However, without the collective effort of researchers, clinicians, and engineers, the transformative potential of this technology may languish in theoretical discussions rather than translating into tangible outcomes for those who need it most.
In conclusion, the journey to integrate crystal phase change materials into neonatal intensive care presents a landscape rich with potential yet fraught with challenges. It calls for ongoing interrogation of existing methodologies, a commitment to rigorous testing, and a collaborative spirit among diverse disciplines. Ultimately, the aim is to not only warm premature babies with innovative science but also to cultivate a healthcare framework capable of evolving with advancements in research and technology.